Understanding Vulvar Cancer
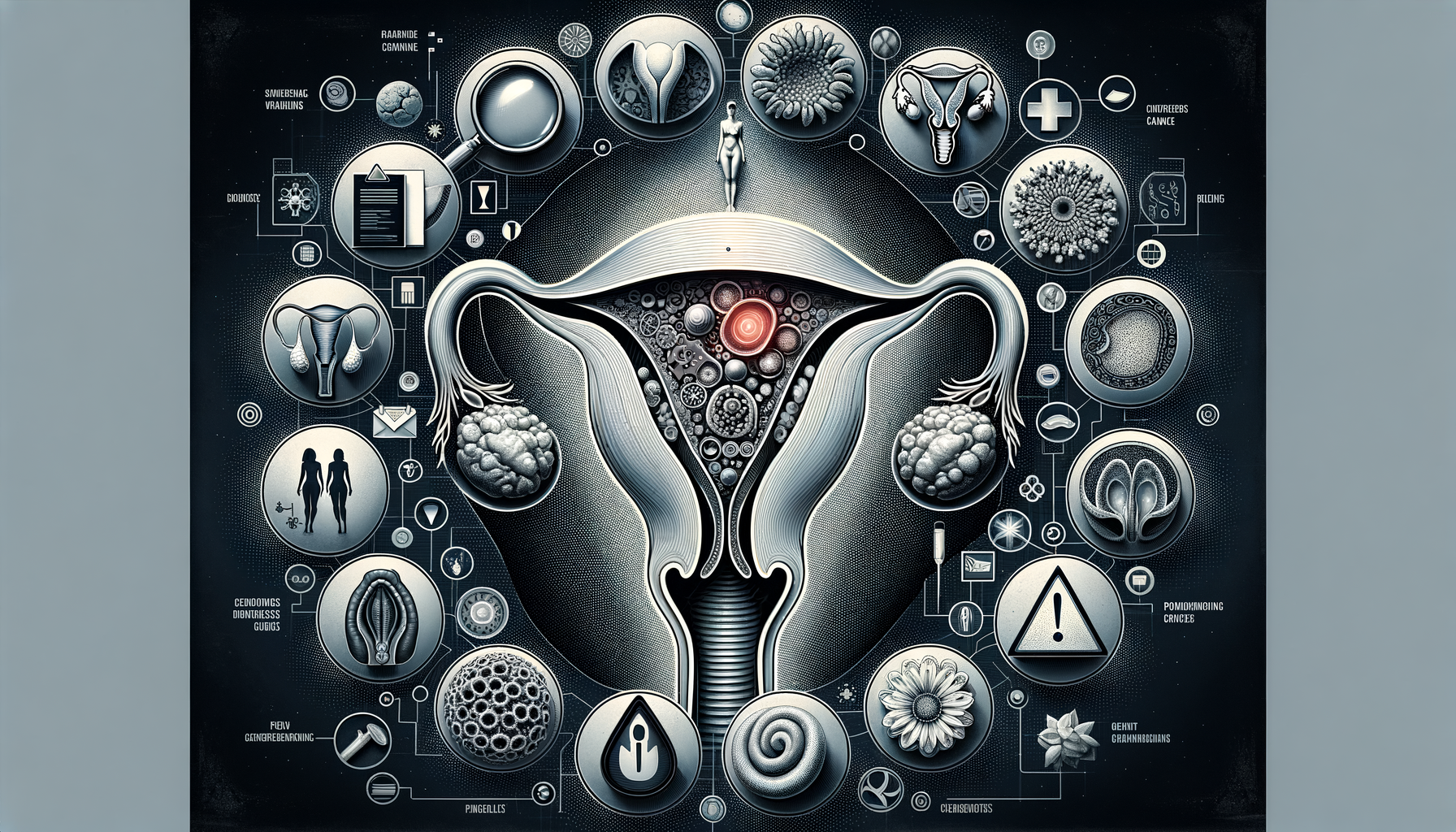
Vulvar cancer is a rare type of cancer that occurs on the external surface area of the female genitalia. Although it represents a small percentage of gynecological cancers, its impact can be significant, affecting a woman’s health and quality of life. Understanding this condition begins with recognizing its nature and how it develops. Vulvar cancer typically affects older women, but it can occur at any age, making awareness of its signs and symptoms crucial for early detection and treatment.
The vulva includes the labia, clitoris, and the opening to the vagina, and cancer can develop in any of these areas. The most common type of vulvar cancer is squamous cell carcinoma, which originates in the flat cells lining the vulva. Other types include melanoma, adenocarcinoma, and basal cell carcinoma. Each type has distinct characteristics and may require different treatment approaches.
Early detection of vulvar cancer significantly increases the chances of successful treatment. This makes it essential for women to be aware of the early warning signs and seek medical advice if they notice any changes. Regular gynecological examinations also play a vital role in detecting abnormalities that could indicate the presence of cancer.
Early Warning Signs to Watch For
Recognizing the early warning signs of vulvar cancer can be lifesaving. The symptoms may vary, but there are common indicators that should prompt a visit to a healthcare provider. One of the most noticeable signs is a persistent itchiness in the vulvar area. While itching can be caused by various benign conditions, when it is persistent and does not respond to typical treatments, it can be a sign of underlying issues, including cancer.
Another symptom to be aware of is the presence of lumps or growths on the vulva. These can appear as wart-like lesions or ulcers and may be accompanied by pain or tenderness. Changes in skin color or texture, such as thickening or the appearance of white, dark, or red patches, can also be indicative of vulvar cancer.
Bleeding or discharge that is not related to the menstrual cycle is another warning sign. Any unusual bleeding should be evaluated by a healthcare professional to rule out cancer or other conditions. Additionally, persistent pain in the pelvic area or during intercourse can be a symptom of vulvar cancer.
Risk Factors and Prevention
Understanding the risk factors associated with vulvar cancer can help in taking preventive measures. Age is a significant risk factor, with most cases occurring in women over 65. However, younger women are not immune, especially if they have certain risk factors. Human papillomavirus (HPV) infection is a major risk factor, as it is linked to many cases of vulvar cancer. Other risk factors include smoking, a history of genital warts, and having a weakened immune system.
Preventive measures include regular gynecological check-ups and HPV vaccination, which can reduce the risk of HPV-related cancers. Practicing safe sex and quitting smoking are also effective strategies in lowering the risk. Women should also be encouraged to perform regular self-examinations to detect any changes in the vulvar area early.
Maintaining a healthy lifestyle with a balanced diet and regular exercise can enhance overall health and potentially reduce cancer risk. Awareness and education about vulvar cancer and its risk factors are key components in prevention and early detection.
Diagnosis and Treatment Options
If vulvar cancer is suspected, a healthcare provider will conduct a thorough examination and may order a biopsy to confirm the diagnosis. Imaging tests, such as MRI or CT scans, might be used to determine the extent of the cancer. Once diagnosed, the treatment plan will depend on the stage and type of cancer, as well as the patient’s overall health and preferences.
Treatment options for vulvar cancer include surgery, radiation therapy, and chemotherapy. Surgery is often the primary treatment and may involve removing the cancerous tissue along with some surrounding healthy tissue to ensure all cancer cells are eliminated. In more advanced cases, lymph nodes in the groin may also be removed.
Radiation therapy may be used alone or in combination with surgery to destroy cancer cells and reduce the risk of recurrence. Chemotherapy is typically reserved for advanced stages or when cancer has spread to other parts of the body. Participation in clinical trials may also be an option for some patients, offering access to new and potentially more effective treatments.
Living with Vulvar Cancer
Being diagnosed with vulvar cancer can be overwhelming, but support and resources are available to help patients and their families navigate this challenging time. Emotional and psychological support is crucial, as the diagnosis and treatment can impact a woman’s body image and self-esteem.
Joining support groups can provide a sense of community and shared experience, helping patients cope with the emotional aspects of the disease. Counseling and therapy services are also beneficial in managing stress and anxiety related to the diagnosis and treatment.
Practical support, such as assistance with daily activities and transportation to medical appointments, can ease some of the burdens associated with treatment. Patients should be encouraged to communicate openly with their healthcare team about any concerns or side effects they experience, as there are often ways to manage these effectively.
Maintaining a positive outlook and focusing on self-care can significantly enhance quality of life during and after treatment. With advances in medical care and ongoing research, there is hope for improved outcomes and a brighter future for those affected by vulvar cancer.



Leave a Reply